Included Content
- Homeostasis
- Membrane Potential I & II
- The Action Potential
- Synaptic Potential
- Autonomic Physiology I, II & III
- Metabolic Fuel Sources in the Fed & Fasting States
- Glycolysis & Pyruvate Dehydrogenase Complex
- TCA Cycle & Anaplerotic Reactions
- ETC, Oxygen Reduction, and Reduce Biochem I & II
- Gluconeogenesis & Glycogen Metabolism
- Cell Death & Differentiation I & II
-
Which of the following is a classic example of a positive feedback physiological response?
- Blood insulin levels
- Heart rate
- Blood pressure and baroreflexes during exercise
- Blood pressure and baroreflexes during rest
- OsmoregulationAnswer C.
Homeostasis.
-
Once a vessel is damaged, platelets start to cling to the injured site and release chemicals that attract more platelets. The platelets continue to pile up and release chemicals until a clot is formed. Blood clotting is an example of:
- Negative Feedback
- Positive Feedback
- High Gain System
- Low Gain System
- None of the aboveAnswer B.
Homeostasis.
-
Orthostatic hypotension occurs when a person’s blood pressure falls when suddenly standing up from a lying or sitting position. It occurs predominantly by delayed constriction of the lower body blood vessels, which is normally required to maintain an adequate blood pressure when changing position to standing. As a result, blood pools in the blood vessels of the legs for a longer period and less is returned to the heart, thereby leading to a reduced cardiac output. This is an example of:
- Negative Feedback
- Positive Feedback
- High Gain System
- Low Gain System
- None of the aboveAnswer D.
Homeostasis.
-
Your friend in medical school asks why depolarizing the membrane (such as in a state of acidemia), eventually leads to fewer action potentials. The best answer is:
- Depolarization makes the cell more permeable to Cl-, which eventually hyperpolarizes the membrane.
- Depolarization has a boomerang effect and eventually leads to hyperpolarization.
- Depolarization, if prolonged, leads to inactivated Na+ channels.
- Depolarization causes degradation of K+ channel proteins
- Did you hear the one about global warming? It depolarizes! Answer C. If the cell membrane is in a depolarized state, at first it reacts more readily to stimuli, because less stimulus is necessary to reach threshold. However, if the cell remains in a depolarized state and cannot reach a high enough membrane potential to reset the Na+ gates, those Na+ will remain inactive and eventually even a strong stimulus will not initiate a strong enough Na+ response, leading to fewer transferred action potentials.
Membrane Potential.
-
Which part of a K+ channel subunit is primarily responsible for K+ selectivity over Na+?
- S5 (outer helix)
- S6 (inner helix)
- P segment
- Alpha binder
- Hyrophospate end Answer C. The P segments form the “selectivity filter”.
Membrane Potential.
-
A patient is diagnosed with hypoxia, which of the following is NOT true about the patient with regard to membrane potentials in B cells of the pancreas?
- ATP sensitive K+ channels are open
- Voltage sensitive Ca2+ channels are open
- Insulin is not being secreted
- The membrane is hyperpolarizing
- Vm is increasing Answer C.
Membrane Potential.
- A patient comes in with CO poisoning. What can be said about the likelihood (at first) of membrane threshold being reached compared to the normal?
- The cell is depolarized, it is more likely to reach threshold.
- The cell is hyperpolarized, it is more likely to reach threshold.
- The cell is depolarized, it is less likely to reach threshold.
- The cell is hyperpolarized, it is less likely to reach threshold. Answer A. CO poisoning reduces the amount of O2 being dropped off in cells, this means that OXPHOS is less active and that less ATP is being generated. Less ATP = less K+Na+ATPase running. Less ATPase running = positive charge building up on the inside of the cell. Positive charge buildup intracellularly = depolarization. Depolarization = more likely to reach threshold.
NOTE: after the cell reaches threshold, some of the Na+ channels don’t reset, because the cell doesn’t reach a negative enough voltage to reset them, rendering them inactive. At this point, the remaining gates have difficulty creating a strong enough flow of ions to transfer the signal, so the membrane become LESS reactive to stimulus. However, AT FIRST the depolarization makes it easier to reach threshold.
Membrane Potential.
-
Which of the following is correct in regards to graded potentials and action potentials?
- Graded potentials (GP) occur in the axon hillock; action potentials (AP) occur in the dendrites/cell bodies
- GP and AP can both only be depolarized
- AP can be initiated with above threshold graded potentials at axon hillock; GP are initiated in ions through channels
- GP only occur with voltage gated ion channels; AP can occur with any type of ion channel
- AP always have the same strength of signal and have a refractory period that must be obeyed; GP cannot have summation Answer C.
The Action Potential.
-
Which of the following is true regarding the conductance velocity of an action potential?
- Myelin decreases conduction velocity by providing insulination for the axon
- Axons with smaller diameters have increase conduction velocity
- Preganglionic fibers often have a slower conduction velocity as compared to postsynaptic fibers since they are unmyelinated
- Myelination decreases capacitance by allowing action potentials to “jump” from node to node, increasing conduction velocity
- Myelination creates a greater surface area to allow for ion exchange across membranesAnswer D.
The Action Potential.
-
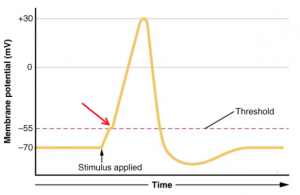
Which of the following is occurring at the point in the graph depicted by the red arrow?

- Na+ activation gates are open
- Na+ inactivation gates are closed
- K+ activation gates are closing
- K+ inactivation gates are opening
- None of the aboveAnswer A.
The Action Potential.
-
A neuron has a threshold of -45 mV. Resting membrane potential is -60 mV. A depolarization stimulus of 10 mV is applied. What is the effect?
- There will be no effect
- The neuron will depolarize however an action potential will not fire
- An action potential will fire
- The neuron will hyper-polarize
- Initially, the neuron will hyperpolarize but then it will depolarize Answer B.
The Action Potential.
-
When there is an increased stimulus, there is an increased frequency in action potential firing. What are some of the effects this could have?
- Greater neurotransmitter release from axon terminal which causes a greater target response
- Change in amplitude of the action potential
- Increased acetylcholine release in synaptic cleft causing a greater depolarization of cell to cause more frequent firing and greater calcium release
- A, B
- A, CAnswer E. Action potentials have the same morphology (same amplitude) even when there is an increased firing of action potentials. The morphology of an action potential does however change when the upstroke of action potentials changes as the threshold for firing an action potential decreases and RRP progresses. An increased stimulus causing more acetylcholine to be released which causes more frequent firing and more calcium release from the cell to allow for more muscle contraction.
The Action Potential.
-
An action potential can serve many functions in the body, what are some of the effects of blocking an action potential?
- Cellular response to allow for muscle contraction and neurotransmitter release
- Blocking in sensory nerves can allow for analgesic effects
- Information delivery to the central nervous system
- The cell will always remain depolarized Answer B. A drug example would be lidocaine which is a fast sodium blocker and allows for local analgesic effects since it is working on blocking action potentials in sensory nerves over a small diameter.
The Action Potential.
-
You have been having troubles lately and your OMS1 friend decides to play doctor and suggest that you seek out some natural sources for Serotonin, postulating that this will help you sleep and feel better. Of her suggestions, which one could lead to more serotonin?
- Tyrosine in a supplement from Walmart.
- Glutamate that is in MSG and can be gotten at Harps.
- Choline which she swears is sold by the pound at the Farmer’s Market on Saturday.
- Dopa decarboxylase that is sold on the corner near the riverfront.
- Tryptophan which is in turkey, they are on sale at Aldi. Answer E.
Synaptic Physiology.
-
Metoprolol is a beta 1 blocker often given to patients with high blood pressure. Patients who are prescribed this medication often stop taking it because of annoying side effects. What other side effect can be contributed to the beta 1 blocking ability of Metoprolol.
- Excess sweating
- Weight gain
- Bronchiolar constriction
- Rashes
- Dry eyes Answer B. Beta one blockers work against lipolysis and patients often have weight gain and inability to easily lose weight.
Synaptic Physiology.
-
In a neuron where potassium channels are inappropriately opened, what will be the effect on the excitability of the neuron.
- It will be unaffected because the Na/K pumps are still working.
- It will be more excitable due to depolarization.
- It will be less excitable due to hyperpolarization.
- The potassium channel will reset before any effect can be noticed.
- This will cause a chlorine channel to open and balance out the effect.Answer C.
Synaptic Physiology.
- A patient is excreting high levels of VMA (3-Methoxy-4-hydroxymandelic acid) in their urine. This would suggest high levels of which neurotransmitter(s)?
- Epinephrine
- Dopamine
- Norepinephrine
- A & B
- A & C Answer E.
Synaptic Physiology.
-
A neuron fires an action potential. From that we know that:
- The neuron received only excitatory inputs.
- The neuron received only inhibitory inputs.
- The neuron received a balance of excitatory inputs and inhibitory inputs but that the excitatory inputs were closer to the axon hillock.
- The neuron received enough excitatory inputs to fire an action potential even if inhibitory inputs were received as well.
- Neurons are magic and they fire when they feel like it. Answer D.
Synaptic Physiology.
-
Alkalosis has a profound effect on neurons. It is most notable in
- States of hypoxia where the low oxygen reduces availability of ATP for the Na/K pumps.
- States of diabetic ketoacidosis which lead to coma.
- Epilepsy where patients will attempt to blow off CO2, hyperventilate, elevate their blood pH and induce seizures
- Cause the neuron to reverse polarity and send all action potentials back up the dendrites to their origins.
- B & D Answer C.
Synaptic Physiology.
-
Denervation supersensitivity describes that after denervation of a cell, the loss of available neurotransmitter causes the cell to…
- Experience necrosis from lack of stimulation
- Become less sensitive to other nerves that innervate it
- Up-regulate receptors, in essence looking for transmitters
- Regrow the nerves from the cell end
- Learn to respond to different neurotransmittersAnswer C.
Synaptic Physiology.
-
During intensive exercise, skeletal muscle metabolites are released in high amounts into the bloodstream. If unchecked, these metabolites would cause a bottoming out of blood pressure. What mechanism is in place that keeps a check on these products, stabilizing blood pressure?
- Sympathetic stimulation of α1 receptors
- Sympathetic stimulation of β2 receptors
- Parasympathetic stimulation of M2 receptors
- Sympathetic stimulation of α2 receptors
- Sympathetic stimulation of β1 receptorsAnswer A.
Synaptic Physiology.
-
In someone infected by the Clostridium botulinum bacteria, there is a complete blockade of a key neurotransmitter to the respiratory muscles. By what means does the botulinus toxin produce this fatal effect?
- Blocking the acetylcholine receptors at the motor plate
- Blocking the release of acetylcholine at the presynaptic terminals
- Inhibiting the action of acetylcholine esterase
- Depletion of acetylcholine at the presynaptic terminal
- Inhibition at the site of the postsynaptic muscarinic receptorsAnswer B.The mechanisms listed are for the following neurotransmitter disruptors:
A – Curare
C – Neostigmine
D – Hemicholinium
E – Atropine
Synaptic Physiology.
-
After determining that your patient has pheochromocytoma, a tumor of the adrenal medulla, you order a urine test expecting elevated levels of metabolites for primarily which small molecule neurotransmitter?
- Nitric oxide
- Acetylcholine
- Norepinephrine
- Epinephrine
- Dopamine Answer D. Note that nitric oxide is a distractor, and is not actually considered to be in the “small molecule” class of neurotransmitters.
Synaptic Physiology.
-
The market for antidepressants and antipsychotics in the pharmaceutical industry is massive, with many drugs targeting the serotonergic synapse. Which of the following would be a viable method for relieving the symptoms of depression at this site?
- Upregulating the expression of monoamine oxidase (MAO)
- Consuming a diet low in tryptophan
- Inhibition of pre-synaptic 5-HT storage
- Inhibition of re-uptake by monoamine transporters
- Selective deactivation of the 5-hydroxytryptophan decarboxylase enzyme Answer D.
Synaptic Physiology.
-
Albuterol is a commonly used beta 2 agonist. What physiological effect with occur upon treatment with albuterol?
- Constriction of vascular smooth muscle
- Dilation of bronchiolar smooth muscle
- Inhibition of adenylyl cyclase
- Decrease in heart rate
- Increased sweat productionAnswer B.
Autonomic Physiology.
-
The autonomic nervous system has many global targets across both sympathetic and parasympathetic pathways. Which of the following is dually innervated by both of these divisions?
- Arteriolar smooth muscle
- Sweat glands
- Cardiac muscle
- Coagulation cascade
- KidneysAnswer C.
Autonomic Physiology.
-
Emily is a 62-year-old obese female BP=186/92, resting HR=72 bpm. She is a very sedentary, non-smoker. You diagnose her with hypertension. As her primary care physician, you prescribe the beta-1 antagonist metoprolol for treatment of her condition. Metoprolol will help lower Emily’s blood pressure through all of the following EXCEPT?
- Heart: decreased heart rate
- Kidney: decreased renin release
- Arterioles: decreased arteriolar vasoconstriction
- Kidney: decreased water conservation
- Heart: decreased force of contraction Answer C. Someone asked why metoprolol is a Beta-1 blocker as oppose to Beta-2. It’s true that B2 receptors control arteriolar vasoconstriction, and thus blood pressure. However, B1 receptors also have a role in blood pressure through their control of the heart and fluid retention in the kidney. We haven’t learned this yet but blood pressure, heart rate, fluid volume, and force of contraction are all interrelated. If your heart rate and force of contraction decrease, so will blood pressure. If you are retaining less fluid, your blood pressure decreases. For example, individuals undergoing hypovolemic shock (low blood volume due to dehydration, hemorrhage, etc) will have an extremely low blood pressure when uncompensated.
Autonomic Physiology.
-
With extreme parasympathetic stimulation present in situations like organophosphate poisoning, you would expect which symptoms to be ABSENT?
- Extreme salivation
- Defecation
- Muscle spasm
- Miosis
- Increased cardiac force of contraction. Answer E.
Autonomic Physiology.
-
Stimulants, colloquially referred to as “uppers,” are drugs that increase activity of the central nervous system by eliciting sympathomimetic effects. Which of the following is most likely a symptom of someone who had taken a stimulant?
- Miosis
- Decreased heart rate
- Profuse sweating
- Increased digestion
- Reduced blood pressure Answer C. Stimulants would cause an increase in the activity of the sympathetic nervous system leading to an increased heart rate, sweating, mydriasis, and increased blood pressure. Inhibition of the sympathetic nervous system would cause increased digestion and decreased heart rate.
Autonomic Physiology.
-
While epinephrine by nature has a global effect on several sympathetic adrenergic receptors, upon its initial release, to which receptor type with it bind to preferentially?
- α1
- α2
- β1
- β2
- β3Answer D.
Autonomic Physiology.
-
Which of the following is true regarding the organization of the autonomic nervous system?
- Somatic motor neurons have a large diameter, allowing for them to conduct action potentials faster
- Sympathetic preganglionic fibers are long, myelinated fibers that synapse with postganglionic fibers extremely close to the target organ
- Arteriolar smooth muscle is only innervated by the Parasympathetic nervous system
- N2 receptors are located at the neuromuscular junction
- Postganglionic fibers are usually unmyelinated and thus conduct action potentials at a slower rate Answer E.
Autonomic Physiology.
-
Caffeine is a potent inhibitor of phosphodiesterase. Considering this, in which of the following might caffeine have a stimulatory effect?
- Sweat glands
- Vascular smooth muscle
- Presynaptic sympathetic nerve terminals
- Sympathetic ganglion
- CardiomyocytesAnswer E.
Autonomic Physiology.
-
Tonic control regulates physiological parameters in an up-down fashion. Match the effects of the neurotransmitter and the correct nervous system with its associated physiological effect.
- Increased acetylcholine would be present for the parasympathetic nervous system and cause vasoconstriction and therefore hyperventilation
- Decreased norepinephrine for the sympathetic nervous system would cause a decrease in signal rate and therefore blood vessel dilation to cause an increase in blood pressure
- Decreased norepinephrine for the sympathetic nervous system would cause a decrease in signal rate and therefore blood vessel dilation to cause a decrease in blood pressure
- Increased acetylcholine would be present for the sympathetic nervous system and cause vasoconstriction and therefore hypoventilation
- Increased norepinephrine for the sympathetic nervous system would cause a decrease in signal rate and therefore blood vessel dilation to cause a decrease in blood pressureAnswer C.
Autonomic Physiology.
-
You are doing rotations in the Emergency Department when a 25-year-old female patient is brought in via ambulance. The paramedics tell you that she is in anaphylaxis due to a bee sting. You’re a super smart med student, so you know that anaphylactic shock is associated with systemic vasodilation that causes low blood pressure. Which of the following would be the best course of action in order to fix this associated vasodilation and drop in blood pressure?
- You should administer a high dose of epinephrine since α-receptors have a lower affinity for Epinephrine than that of ß-receptors.
- You should administer a high dose of Epinephrine since α-receptors have a higher affinity for Epinephrine than that of ß-receptors.
- You should administer a low dose of epinephrine since α-receptors have a lower affinity for Epinephrine than that of ß-receptors
- You should administer a low dose of epinephrine since α-receptors have a higher affinity for Epinephrine than that of ß-receptors
- You should administer Viagra Answer A.
Autonomic Physiology.
-
Which branch of the nervous system is the best at quickly conducting signals to its effectors?
- Somatic motor
- Autonomic sympathetic adrenergic
- Autonomic sympathetic muscarinic
- Autonomic sympathetic cholinergic
- Autonomic parasympathetic muscarinicAnswer A. Somatic motor neurons are fully myelinated all the way to the skeletal muscle. No other nervous system branch is fully myelinated.
Autonomic Physiology.
-
Which division of the autonomic nervous system has the shortest postganglionic distance?
- Nicotinic 1 motor plate
- Sympathetic cholinergic
- Sympathetic muscarinic
- Parasympathetic muscarinic
- Parasympathetic cholinergicAnswer D.
Autonomic Physiology.
-
The ganglionic blocking drug hexamethonium, which antagonizes N2 receptors, is administered intravenously. Which of the following would be most likely to be observed in response to administration of this drug?
- Tachycardia, increased blood pressure
- Bradycardia, decreased blood pressure
- Tachycardia, decreased blood pressure
- Tachycardia or bradycardia equally likely, decreased blood pressure
- Tachycardia or bradycardia equally likely, increased or decreased blood pressure also equally likelyAnswer D.
Autonomic Physiology.
- Vagal maneuvers involve various techniques of stimulating the vagus nerve (CN X) in order to elicit a specific response in the autonomic nervous system. For example, health care providers may trigger the gag reflex in their patient to stimulate this nerve and provide a therapeutic effect. Which of the following is most likely the intended effect of a vagal maneuver?
- Decrease heart rate
- Bronchodilation
- Decrease gut motility
- Increase sweat production
- Miosis Answer A. The Vagus nerve (also known as CN X) is responsible for parasympathetic innervation of the heart, lungs, and gut. It’s involved in slowing heart rate, bronchoconstriction, and increasing gut motility. Vagal maneuvers are often used in patients exhibiting tachycardia.
Autonomic Physiology.
-
Ahsan, a mentally exhausted medical student, decided to take a study break and go for a hike at Devil’s Den. He accidentally travelled off the beaten path when he heard some unusual noises coming from the brush. Luckily Ahsan is a highly trained eagle scout and recognized the sounds immediately as the call of a cougar. He sprung into action, boldly running from the noise and flooding his body with adrenaline. Assuming that Ahsan had eaten a meal high in carbohydrates within an hour of this occurrence, which of the following is true?
- Epinephrine will activate a tyrosine kinase receptor signaling pathway causing the breakdown of Glycogen.
- His high BGL would trigger a release of Insulin and the dephosphorylation of Glycogen Synthase by Protein phosphatase.
- Glucagon would be released causing the activation of PKA and the subsequent dephosphorylation of Glycogen synthase and phosphorylase kinase.
- Despite his high BGL, Epinephrine will work in a similar manner to that of Glucagon causing the phosphorylation of Glycogen synthase and Glycogen phosphorylase.
- Epinephrine will activate a similar signaling cascade to that of Insulin, causing an activation of PKB (Akt) and subsequent phosphorylation of Glycogen synthase. Answer D. Epinephrine is involved in a similar signaling pathway to that of Glycogen. However, instead of activating PKA, it activates PKC and calmodulin via the release of Ca2+. This leads to the phosphorylation of Glycogen synthase (inactivating it) and Phosphorylase kinase (activating it). Despite Ahsan’s high BGL, Epinephrine will inhibit the buildup and activate the breakdown of Glycogen in order to provide the energy needed to escape the cougar.
Metabolic Fuel Sources in the Fed and Fasting States.
-
After consuming glucose, insulin production is turned on, whereas glucagon is turned off. Which of the following is true in the fed state?
- Glycogen synthesis is inhibited by the increase in insulin.
- Fatty acid synthesis is inhibited by glucagon to maintain blood glucose levels.
- Lactate production is increased, resulting in an increase in glycogen synthesis.
- Fatty acids are broken down to maintain blood glucose levels.
- Glycogen synthesis is stimulated by insulin and stored in the liver and skeletal muscle.Answer E.
Metabolic Fuel Sources in the Fed and Fasting States.
-
A patient has bloodwork done two hours after consuming a sugary drink. Since consuming the drink, the patient has consumed no other food or beverages. The patient’s blood glucose level is 163 mg/dL. What can be said about the patient?
- The patient’s results are considered normal.
- The patient is considered pre-diabetic.
- The patient is considered diabetic.
- The patient is not producing insulin.
- Cannot determine with the information provided.Answer B. After two hours, normal levels of blood glucose are <140 mg/dL, pre-diabetic levels are between 140-200 mg/dL, and diabetic levels are >200 mg/dL. Metabolic Fuel Sources in the fed and fasting states.
-
Pig insulin was regularly administered to diabetic patients before the structure of human insulin was discovered. Now that the structure is known, doctors are able to administer the active portion of insulin, while still being able to measure the amount of insulin being produced by the body. Which part of human-secreted insulin is measured?
- A-chain
- B-chain
- Proinsulin
- C-peptide
- InsulinAnswer D. The C-peptide is the portion of proinsulin that is cleaved to activate insulin. Insulin that is administered to patients does not include the C-peptide; it only contains the active portion of the hormone (A-chain and B-chain).
Metabolic Fuel Sources in the fed and fasting states.
-
You are on a pediatrics rotation when a 5-year-old female patient is brought into the clinic by their mother. The patient is severely obese. However, the mother mentions that her daughter’s nutrition is good but she is constantly hungry. What is the next thing you should do?
- Refer them to a nutritionist
- Test for a Leptin deficiency
- Test for AMPK deficiency
- Test for brain damage within the hypothalamus
- Test for Type I Diabetes mellitusAnswer B.
Metabolic Fuel Sources in the fed and fasting states.
-
The X-linked genetic disorder known as Leigh disease presents with mortally high levels of lactic acid in the blood due to a PDH E1 defect. With this disorder, the PDH E1 subunit would most likely display difficulty binding to which essential coenzyme?
- FAD
- Lipoate
- TPP
- Lipoamide
- PantothenateAnswer C.
Glycolysis and Pyruvate Dehydrogenase.
-
The glycolytic enzyme PFK-1 would have decreased function under which of the following conditions?
- High concentrations of ATP
- High concentrations of AMP
- High concentrations of F-2,6-BP
- Low concentration of citrate
- Mutation resulting in decreased activity at the ATP effector binding site Answer A.
Glycolysis and Pyruvate Dehydrogenase.
-
Which of the following is an activator of pyruvate kinase in the liver?
- Alanine
- ATP
- GTP
- Fructose-1,6-P
- None of the aboveAnswer D.
Glycolysis and Pyruvate Dehydrogenase.
-
The activity of pyruvate dehydrogenase complex is a crucial process in carbohydrate metabolism which is regulated by the activity of two enzymes. What would you expect to see in a patient with a deficiency in the PDC kinase enzyme?
- Increased activity of pyruvate dehydrogenase complex compared to a person with normal amount of PDC kinase enzyme
- Decreased activity of pyruvate dehydrogenase complex compared to a person with normal amount of PDC kinase enzyme
- No change in the activity of pyruvate dehydrogenase complex compared to a person with normal amount of PDC kinase enzyme
- None of the aboveAnswer A. Without the normal function of PDC kinase, pyruvate dehydrogenase complex will remain active for longer periods of time.
Glycolysis and Pyruvate Dehydrogenase.
-
Which glycolytic intermediates have sufficient energy to drive the production of ATP via substrate level phosphorylation?
- G6P and dihydroxyacetone phosphate
- 1,3-bisphosphoglycerate and phosphoenolpyruvate
- 2-phosphoglycerate and F16-bisphosphate
- F1P and pyruvate
- Glyceraldehyde 3-phosphate and 3-phosphoglycerateAnswer B.
Glycolysis and Pyruvate Dehydrogenase.
-
After consuming a high carbohydrate meal, your body begins to break down and take in the glucose from the meal and you are considered to be in the fed state. Which of the following occurs ONLY in the liver?
- PFK1 activity decreases in response to an increased amount of ATP & citrate
- Hexokinase activity decreases in response to increased amount of G-6-P in the cell
- Pyruvate kinase activity decreases in response to increased amount of ATP and alanine
- Production and storage of glycogen
- Both C and DAnswer C.
Glycolysis and Pyruvate Dehydrogenase.
-
The conversion of Pyruvate to Acetyl CoA is regulated by all of the following EXCEPT:
- Acetyl CoA
- FADH2
- NADH
- NAD+
- CoASHAnswer B.
Glycolysis and Pyruvate Dehydrogenase
- Following extreme trauma, the body would use which TCA intermediate to replace lost heme?
- Oxaloacetate
- Citrate
- Alpha-ketoglutarate
- Succinyl CoA
- SuccinateAnswer D.
TCA Cycle & Anaplerotic Reactions.
-
Wernicke-Korsakoff syndrome is a neurological disorder characterized by mental confusion, amnesia (a permanent gap in memory), and impaired short-term memory. Which of the following enzymes would have reduced function due to this disorder?
- Pyruvate carboxylase
- Lactate Dehydrogenase
- Pyruvate Dehydrogenase
- Malonate Dehydrogenase
- Methylmalonyl-CoA mutase Answer C. Pyruvate DH and alpha-ketoglutarate both require Thiamine (B1), the vitamin deficient in Wernicke-Korsakoff and Beriberi disease. A deficiency in B12 could cause dysfunction in methylmalonyl-CoA mutase while a deficiency in Biotin (B7) could cause dysfunction for Pyruvate carboxylase. Also remember that Pellagra is caused by a deficiency in Niacin (B3).
TCA Cycle & Anaplerotic Reactions.
-
A patient comes to your office with kidney and liver failure. You suspect that methylmalonic acidemia might be their diagnosis which would mean that they are likely deficient in which of the following enzymes?
- Vitamin B1
- Vitamin B2
- Vitamin B3
- Vitamin B5
- Vitamin B12 Answer E.
TCA Cycle & Anaplerotic Reactions.
-
Which of the following is a anapleurotic reaction that occurs in the TCA cycle?
- Aspartate→ Oxaloacetate
- Succinyl CoA→ Heme
- Citrate → Fatty Acids
- Glutamate→ citrate
- Lysine→ SuccinateAnswer A. Anapleurotic reactions are those that replace intermediates in the TCA cycle. Succinyl CoA → Heme is a catapleurotic reaction (pulls succinyl CoA out of the cycle and changes it to something else) as is citrate→ fatty acids.
TCA Cycle & Anaplerotic Reactions.
-
Which of the following is true regarding succinate dehydrogenase?
- It requires Vitamin B1 (Thiamine)
- It oxidizes NADH → NAD+
- It is involved in both the ETC and TCA cycle
- It requires Vitamin B7 (Biotin)
- It produces GTP in its reaction of succinate → fumarateAnswer C. Succinate dehydrogenase also participates as Complex II in the ETC.
TCA Cycle & Anaplerotic Reactions
-
Alcoholics typically have markedly diminished function of pyruvate dehydrogenase and alpha-ketoglutarate dehydrogenase due to decreased dietary absorption of:
- Thiamine
- S-adenosyl methionine
- Succinate
- Riboflavin
- Biotin Answer A.
TCA Cycle & Anaplerotic Reactions.
-
What unique property of non-alpha tocopherols makes them an essential part of a good diet?
- Its higher favorability for oxyradicals
- Its ability to inhibit COX, 5LOX and RNS
- Its higher concentration in tissues than alphaT
- Collaborative function with ascorbate
- The ability to neutralize toxic NAPQI Answer B.
ETC, Oxygen Reduction, and Reduce Biochem.
-
Damage to the ETC by means of cyanide poisoning would lead to leakage of electrons through which channels?
- Complex I
- Complex II
- Complex III
- Complex IV
- Complex I and IIIAnswer E. While CN- does cause lesions of Complex IV, Doctor Hensley explicitly said in the Monday Q&A that damage to complex IV would actually just cause a backup and leakage from I and III, not IV itself.
ETC, Oxygen Reduction, and Reduce Biochem.
-
When there is a bloodborne infection, cells of the immune system produce vast amounts of nitric oxide to destroy the pathogen. This dilates blood vessels and can cause blood pressure to plummet – a condition called septic shock. Which of the following is an additional reason for why an accumulation of NO could be dangerous?
- Excess amounts of nitric oxide can react with superoxide radicals forming peroxynitrite (ONOO-)
- Excess amounts of nitric oxide can react with free oxygen radicals forming peroxynitrite (ONOO-)
- Peroxynitrites (ONOO-) can break down into Nitrogen dioxide radicals (•NO2) and hydroxyl radicals (•OH)
- A & C
- B & CAnswer D.
ETC, Oxygen Reduction, and Reduce Biochem.
-
As a third year medical student, your resident shows you a patient file showing a confirmed diagnosis of chronic granulomatous disease, which is caused by an enzyme mutation in NOX-2. Where is this enzyme located that it would lead to symptoms associated with this condition?
- The inner mitochondrial membrane
- The outer mitochondrial membrane
- Intracellular phagosome membrane
- Extracellular membrane
- This is cause by a free enzyme in the cytosolAnswer C. Chronic granulomatous disease is caused by a mutation in NOX 2, causing the inability to phagocytose and kill bacteria. NOX2 is found in the phagosome membrane of macrophages.
ETC, Oxygen Reduction, and Reduce Biochem.
-
Ischemic strokes occur when the arteries to your brain become narrowed or blocked, causing severely reduced blood flow. Which of the following best describes how a patient’s ETC would be affected if they were experiencing a stroke?
- The lack of blood flow would directly inhibit the function of Complex I and cause a subsequent release of reactive oxygen species from Complex I
- The lack of blood flow would directly inhibit the function of Complex III and cause a subsequent release of reactive oxygen species from Complex I and III
- The lack of blood flow would directly inhibit the function of Complex IV and a subsequent release of reactive oxygen species from Complex I and III
- The lack of blood flow would directly inhibit the function of Complex IV and cause a subsequent release of reactive oxygen species from Complex I and II
- The lack of blood flow would directly inhibit the function of Complex II and cause a subsequent release of reactive oxygen species from Complex I and IIAnswer C.
ETC, Oxygen Reduction, and Reduce Biochem.
-
You are on rotations in an underserved primary care clinic when you come across a patient who can’t stop talking about the importance of antioxidants. They tell you that they researched it on “the Google machine” and that they know all there is to know about antioxidants. When asked, the patient revealed that they’ve been taking Vitamin E for the past 5 years in order to rid their body of reactant radicals. What should you tell them?
- Keep doing what they’re doing, Vitamin E is a great source of alpha-tocopherol which is important in ridding the body of radicals
- They are mistaken and should actually be taking Vitamin D to get the effect they’re wanting
- Keep doing what they’re doing, Vitamin E is a great source of gamma-tocopherol which is important in ridding the body of radicals
- While Vitamin E is a great source of gamma-tocopherol, it doesn’t include the other “non-gamma” tocopherols which are also important in ridding the body of free radicals
- While Vitamin E is a great source of alpha-tocopherol, it doesn’t include the other “non-alpha” tocopherols which are also important in ridding the body of free radicals Answer E.
ETC, Oxygen Reduction, and Reduce Biochem.
-
You are doing clinical rotations in the Emergency Department when a patient comes in who had overdosed on Aspirin. Their symptoms include hyperventilation, vomiting, dehydration, double vision, fever, and feeling faint. A resident asks you to explain the reasoning for why this patient is exhibiting a fever. What are you going to tell them?
- High dose aspirin works as a chemical uncoupler, producing excess heat with the associated energy release
- The fever due to the body’s immunological response to the overabundance of Aspirin
- Aspirin activates UCP1 causing thermogenesis and dissipation of heat from brown adipose stores
- The body creates a fever in order to provide a more suitable environment for the enzymes responsible for metabolizing the Aspirin
- The patient probably has an associated infection.Answer A.
ETC, Oxygen Reduction, and Reduce Biochem.
-
Which of the following is considered to be the most dangerous reactive oxygen species (ROS)?
- Superoxide radical
- Hydrogen peroxide
- Hydroxyl radical
- Hydroxide ion
- Oxygen Answer C.
ETC, Oxygen Reduction, and Reduce Biochem.
-
Hemochromatosis is a disease in which too much iron builds up in your body. The fenton reaction explains why this buildup of iron can be so dangerous. Which of the following best describes the Fenton reaction?
- Fe2+ can react with hydrogen peroxide, producing hydroxyl radicals
- Fe2+ can react with other metals such as Cu+ to produce hydroxide
- Fe2+ can react with free oxygen, producing superoxide radicals
- Fe2+ can react with hydrogen peroxide, producing superoxide radicals
- Fe2+ can react with free oxygen, producing hydroxideAnswer A. Also remember that Wilson’s disease (buildup of Cu+ in the body) would be associated with the Haber-Weiss reaction.
ETC, Oxygen Reduction, and Reduce Biochem.
-
Which enzyme in carbohydrate metabolism works as a tight control point for both the anabolic and catabolic pathways, ensuring that glycolysis and gluconeogenesis are not both active at the same time?
- FBPase-1
- PFK-2
- G-6-Pase
- Pyruvate carboxylase
- PhosphoglucomutaseAnswer B.
Gluconeogenesis & Glycogen Metabolism.
-
Which of the following enzymes is involved in a reaction unique to gluconeogenesis?
- Phosphoglucose isomerase
- Phosphoglyceromutase
- Pyruvate carboxylase
- Phosphofructokinase-1
- Phosphoglycerate kinase Answer C.
Gluconeogenesis & Glycogen Metabolism.
-
Von Gierke disease, is the most common of the glycogen storage diseases. This genetic disease impairs the ability of the liver to produce free glucose from glycogen and from gluconeogenesis. A deficiency in which of the following enzymes would lead to this disease?
- PEPCK
- Glucose-6 Phosphatase
- Pyruvate carboxylase deficiency
- PFK-1
- 2,3-BPG mutaseAnswer B.
Gluconeogenesis & Glycogen Metabolism.
-
For a combination of reasons, high consumption of alcohol leads to a depletion of which carbohydrate metabolite?
- Pyruvate
- Glycogenin
- Oxaloacetate
- 3-phosphoglycerate
- 1,2-bisphosphoglycerateAnswer A.
Gluconeogenesis & Glycogen Metabolism.
-
Lauren, an OMS I student, is celebrating her outstanding performance on the anatomy exam by hitting the dance floor at the Electric Cowboy (she’s got Flossing down!). She realizes that she forgot to eat dinner, but doesn’t want to leave to grab a meal. She opts to pile on the drinks because, after all, alcohol has carbohydrates and she’ll be satisfied (at least for a little bit). How will her body respond?
- Lowering the activity of aldehyde dehydrogenase
- Increasing gluconeogenesis
- NADH levels will decrease but rapidly start increasing
- Initial hyperglycemia, but soon her body will become hypoglycemic
- Initial hypoglycemia, but soon her body will become hyperglycemic Answer D.
Gluconeogenesis & Glycogen Metabolism.
-
Glucagon signaling will do which of the following in the target cell?
- Decrease cAMP levels
- Activate protein phosphatase-1
- Deactivate glycogen phosphorylase-a
- Increase glucose-1-phosphate levels
- Lower 5′-AMP levelsAnswer D.
Gluconeogenesis & Glycogen Metabolism.
-
How much time does it take for glycogen to be depleted?
- 4-5 hours
- 12-14 hours
- 24-36 hours
- 1-2 days
- Glycogen is never depleted since the breakdown of all fuel sources contributes to glycogen storesAnswer B.
Gluconeogenesis & Glycogen Metabolism.
- In preparation for board game night, Seth and Ed each brought their favorite snacks to enjoy throughout the night. Shortly after eating all of his doughnuts, Seth was already hungry again. Ed, however, was still feeling quite content after eating his quinoa and mushrooms. What is the likely cause for this discrepancy?
- The fructose content in Ed’s quinoa was converted to fat, which has twice the calories of carbs, it’s simple science.
- Seth’s doughnuts have a high glycemic index, causing a large, but short spike in blood glucose
- Seth’s doughnuts absorb at a slower rate, so he isn’t getting as much energy from them
- Ed’s quinoa has a high glycemic index, causing a prolonged spike in blood glucose
- Seth’s donuts had a high abundance of Fructose, causing glycolysis to occur unchecked and create an abundance of ATPAnswer B. Answer E is the distractor. They said in class that ATP is highly regulated, therefore Fructose won’t cause an abundance of ATP rather it will just be converted to fat.
Carbohydrate metabolism.
- Angel waddles into class one morning complaining of intense bum soreness that she says is from her CrossFit “workout” the previous evening. This soreness is in part due to the accumulation of lactate. Which of the following best explains the reasoning for why there is an accumulation of lactate during heavy intense exercise?
- Lack of oxygen availability
- Pyruvate is being generated at a higher rate than it can enter the TCA cycle
- Lactate is necessary to perform Gluconeogenesis
- The TCA cycle is inhibited by heavy intense exercise
- The Ca2+ produced from muscle contraction works to upregulate Lactate DHAnswer B.
Carbohydrate Metabolism.
-
Dr. Moffitt is running yet another ultramarathon. As she approaches mile 20, she decides to reach for her gel packet tucked conveniently within her fanny pack in order to get some energy. The gel packet contains a high amount of Fructose. Which of the following is true regarding Dr. Moffitt’s decision to consume this gel packet?
- It’s obviously a mistake, Fructose will be converted to fat which won’t be burned in time to give Dr. Moffitt energy
- Since she is undergoing prolonged exercise, Dr. Moffitt is burning ATP at an high rate and therefore can utilize the Fructose without producing an abundance of fat
- This is a good choice since Fructose will initiate Gluconeogenesis in the liver
- Fructose will undergo glycolysis without being regulated, therefore her consumption of this sugar will lead to an accumulation of fat which can be burned for energy
- A glucose-only gel packet would have given her the same amount of energyAnswer B.
Carbohydrate Metabolism.
- What is TRUE about fructose metabolism?
- It’s the most efficient fuel source for ATP
- Conversion of fructose-1 phosphate to fat is a highly regulated process
- Fructose enters glycolysis after the key regulatory step, allowing it to go unchecked and produce an abundance of fat in the liver
- Regulation of fructose is accomplished by PFK-2, which converts fructose 1-phosphate into fructose 2,6-bisphosphate
- The relatively high ratio of glucose to fructose in high fructose corn syrup is what makes the substance so bad for youAnswer B. E is the distractor. They said in class that ATP is highly regulated, therefore Fructose won’t cause an abundance of ATP rather it will just be converted to fat.
Carbohydrate Metabolism.
- One of your patients is Type II diabetic. In order to help them increase their insulin sensitivity you recommend more frequent exercise which you expect will:
- Lead to higher levels of insulin in the body
- Promote recruitment of more GLUT4 receptors
- Increase skeletal muscle of utilization of insulin during exercise only
- Increase insulin synthesis by pancreatic beta cells
- Decrease skeletal muscle utilization of insulin during rest onlyAnswer B.
Carbohydrate Metabolism.