- A patient presents with tremors, slurred speech, drowsiness, and blurred vision. Suspecting hyperammonemia, you would expect which of the following to be true?
- Low neuronal GLU
- High astrocyte GLU
- Low neuronal PAG
- High astrocyte αKG
- High astrocyte GLNAnswer E.
Amino Acid Metabolism.
- A female neonate appeared healthy until age ~24 hours, when she became lethargic. A sepsis workup proved negative. At 56 hours, she started showing focal seizure activity. The plasma ammonia level was found to be 887 μmol/l (normal 5–35 μmol/l). Quantitative plasma amino acid levels revealed a marked elevation of citrulline but not argininosuccinate. Which enzyme is most likely found to be deficient in this patient?
- Arginase
- Argininosuccinate lyase
- Argininosuccinate synthetase
- Carbamoyl phosphate synthetase I
- Ornithine transcarbamylaseAnswer C.
Amino Acid Metabolism I.
- A patient presents with early onset arthritis in large joints and he states that his urine turns dark after a while. After running a few tests, you diagnose the patient with alkaptonuria. Which treatment options would you provide for you patient?
- Increased intake of phenylalanine and fumarate
- Restricted intake of phenylalanine and tyrosine
- Restricted intake of leucine, isoleucine, and valine
- Increased intake of protein and phenylbutyrate
- Prescribe antibiotics to suppress hyperammonemiaAnswer B.
Amino Acid Metabolism.
- Vitamin B6 is a necessary cofactors in which enzymes:
- Methionine adenosyltransferase and cystathionine lyase
- Cystathionine beta synthase and cystathionine lyase
- Cystathionine beta synthase and dihydrofolate reductase
- Cystathionine lyase and methionine synthase
- Methionine adenosyltransferase and methionine synthaseAnswer B. see transsulfuration pathway.
- Cystinosis is a pediatric illness which can best be treated with:
- Urinary alkalization with citrate
- Acetazolamide
- Cysteamine to form cysteamine-Cys for excretion
- Flurodeoxy-uracil
- Broad spectrum vitamin B supplementationAnswer C. urinary alkalization and acetazolamide are for cystinuria, flurodeoxy-uracil is a cancer treatment that targets DHFR and there is no indication that B supplementation is beneficial.
- Which of the following is TRUE regarding the RBC?
- During a state of starvation, the RBC runs primarily off ketone bodies
- Hemoglobin is taken from the ferric (3+) state to the ferrous (2+) state via the reduction of cytochrome b5
- 2,3 BPG increases the affinity of hemoglobin to bind to oxygen
- NADPH is utilized to oxidize glutathione
- Low oxygen levels trigger the kidney to release Epo, causing an increase in erythopoiesis Answer .
RBC Dynamics.
- Epoetin (Procrit) injection is a man-made version of human erythropoietin (EPO). In which of the following situations would Epoetin be an appropriate medication to give?
- A patient suffering from hemolytic anemia
- A patient suffering from thrombocytopenia
- A patient suffering from hypocalcemia
- A patient suffering from Polycythemia
- A patient suffering from hypokalemia Answer A.
RBC Dynamics.
- You are counseling a 24 year old male patient that has recently found out they are a carrier of the sickle cell trait. Because they are heterozygous, you tell him:
- He has nothing to worry about and will not display any characteristics of sickle cell
- Under conditions of low oxygen, he can manifest symptoms of sickle cell anemia.
- He should avoid areas where malaria is endemic.
- Under conditions of high oxygen, he can manifest symptoms of sickle cell anemia.
- Under the right conditions, the sickling can cause him to enter liver failure. Answer B.
RBC Dynamics.
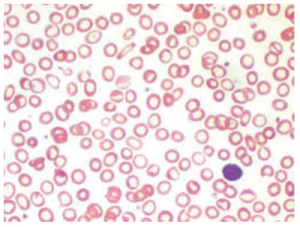
- A 29 year old female patient comes to your clinic complaining of dizziness, fatigue, and lightheadedness. You ask the lab to rub a peripheral blood smear and the results are shown below. Which of the following is the most appropriate differential diagnosis?

- B12 deficiency
- Folate deficiency
- Sickle cell disease
- Internal hemorrhage
- B6 deficiency Answer B. B6 deficiency causes microcytic, hypochromic anemia due to its role in heme synthesis.
RBC Dynamics.
- Ammunol is an FDA-approved intravenous solution of 10% sodium benzoate and 10% phenylacetate used to treat hyperammonemia due to the inability to create urea. Which of the following does this drug aim to deplete in order to rid the body of ammonia?
- Glycine & Glutamate
- Glutamate & Aspartate
- Aspartate & Arginine
- Glycine & Glutamine
- Lysine & Glutamine Answer D. Lecture #57 Synthesis & Catabolism of porphyrins.
RBC Dynamics.
- Angel M. presents to the clinic with symptoms of of nausea/vomiting after habitually licking the wall of her house that was built in 1945. You suspect lead poisoning as the source for her symptoms. Which of the following explains how lead elicits toxic effects?
- Lead inhibits ALA synthase, which is vital for the condensation of succinyl Co-A and Glycine in the production of porphyrin
- Lead degrades B12 which induces symptoms mimicking pernicious anemia
- Lead inhibits delta-ALA dehydratase which is vital for transporting porphyrin precursors into the mitochondria
- Lead inhibits the production of conjugated bilirubin
- Lead replaces iron on heme increasing the affinity of Hb to bind to oxygen, disallowing its release to tissues Answer C.
Synthesis & Catabolism of porphyrins.
- Which of the following is NOT a manner in which heme synthesis is regulated?
- Heme represses the synthesis of delta-ala synthase
- Heme inhibits movement of ala synthase into mitochondria
- Iron controls translation of ala synthase mRNA
- Heme down regulates ALA synthase
- Epo decreases transcription of ala synthase Answer E.
Synthesis & Catabolism of porphyrins.
- A 23 year old female patient presents to the clinic with unusual skin lesions in areas that have been exposed to sunlight. Which of the following is most likely is the underlying disease associated with this symptoms?
- Acute intermittent porphyria
- Porphyria cutanea tarda
- Thrombocytopenia
- Anemia of chronic disease
- Psoriasis Answer B. Remember that acute intermittent porphyria is characterized by episodic acute neurovisceral attacks.
Synthesis & Catabolism of porphyrins.
- A 52 year old male patient presents to the clinic with complaint of yellowing of the skin and eyes. Clinical assay reveals elevated conjugated bilirubin. Which of the following would be a differential diagnosis?
- Bile duct obstruction
- Hepatitis C
- Cirrosis
- Hemolytic anemia
- Internal bleeding Answer A.
Synthesis & Catabolism of porphyrins.
- A 58 year old male presents to the clinic with jaundice. After a full history and physical examination are complete, you decide to order a bilirubin test to get to the bottom of this patient’s jaundice. The results are shown below:
TIBL 2.1 mg/dL (N = 0.3 – 1.0 mg/dL)
Direct Bilirubin 0.1 mg/dL (N = 0.1-0.4 mg/dL)
Which of the following would be the most appropriate differential diagnosis?- The patient has elevated direct bilirubin, indicating cirrhosis, hepatitis, or hemolytic anemia.
- The patient has elevated indirect bilirubin, indicating cirrhosis, hepatitis, or hemolytic anemia.
- The patient has elevated direct bilirubin, indicating a bile duct obstruction
- The patient has elevated indirect bilirubin, indicating bile duct obstruction.
- The patient’s direct bilirubin is within range, showing that the jaundice is not being caused by an excess buildup of bilirubin. Answer B.
Synthesis & Catabolism of porphyrins.
- A 42 year old female presents to the clinic complaining of generalized fatigue. Upon review of her history, you note that she has been previously diagnosed with Rheumatoid Arthritis, a chronic inflammatory disorder. After a full examination, you get have a gut feeling this patient is displaying symptoms of anemia of chronic disease and decide to order a CBC/reticulocyte count. Which of the following best explains the reasoning behind this differential diagnosis?
- Inflammatory disorders are associated with an increase in IL-6 which would increase hepcidin, and decrease circulating iron levels.
- Inflammatory disorders are associated with an increase in IL-6 which would decrease hepcidin, and decrease circulating iron levels.
- Inflammatory disorders are associated with an increase in the number of hypersegmented neutrophils resulting from an overactive immune response.
- Inflammatory disorders are associated with an increase in IL-3 which would increase hepcidin, and decrease circulating iron levels.
- Inflammatory disorders are associated with an increase in IL-3, which would decrease hepcidin, and decrease circulating iron levels. Answer A.
Iron metabolism.
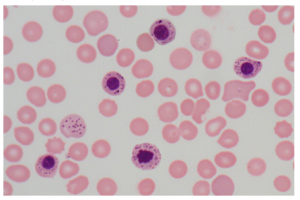
- A 17 year old female presents to the clinic with complaints of constipation, nausea, fatigue and irritability. Laboratory studies include:
Hemoglobin 11.3 g/dL (N = 12- 16)
HCT 25% (N = 37-47)
Erythrocyte count 5.2 million/mm3 (N = 4.2-5.4)
MCV 82 um3 (N = 80-98)
Follow-up laboratory studies show that the serum iron concentration and ferritin are elevated, although TIBC is within reference range. A peripheral smear is performed is shown below. Which of the following in the most likely diagnosis?
- Anemia of chronic disease
- Iron deficiency anemia
- Sideroblastic anemia
- Alpha-thalassemia minor
- Beta-thalassemia minor Answer C.
Iron Metabolism.
- A 25 year old woman has a routine, pre-employment physical examination. Laboratory studies include:
Hemoglobin 11.3 g/dL (N = 12- 16)
HCT 34% (N = 37-47)
Erythrocyte count 5.2 million/mm3 (N = 4.2-5.4)
MCV 65 um3 (N = 80-98)
Follow-up laboratory studies show that the serum iron concentration and iron-binding capacity are within the reference ranges. Hemoglobin electrophoresis shows increased hemoglobin A2. Which of the following in the most likely diagnosis?- Anemia of chronic disease
- Iron deficiency anemia
- Sideroblastic anemai
- Alpha-thalassemia minor
- Beta-thalassemia minor Answer E.
Iron Metabolism.
- Seth B. has just dramatically fallen down the steps of the atrium, cutting his arm and causing profuse bleeding. He is transported to the hospital via ambulance where the ER physician on duty decides that he is in need of a blood transfusion. If Seth B. has the blood type A-, which of the following blood types will be be able to receive via a transfusion?
- O+
- O-
- A+
- A & B
- A, B, & CAnswer B. A- can receive from A- or O-. They can not receive blood from donors that are Rh+.
General Blood Histology & Hemopoiesis.
- You are doing rotations in the Emergency Department, when you come across a patient that has just recovered from an anaphylactic episode after accidentally eating a peanut. Your attending asks you what cells are primarily responsible for producing the effects associated with anaphylaxis. How do you answer?
- Eosinophils and neutrophils
- Neutrophils and Basophils
- Basophils and Mast Cells
- Eosinophils and Basophils
- Neutrophils and Mast Cells Answer C.
General Blood Histology & Hemopoiesis.
- You are doing rotations in the OB-GYN department when you are called to assist with a 32 year old female patient who is approximately 8 months pregnant. The mother’s blood type is O negative, and she is pregnant with her 2nd child that is Rh+. She had her 1st in a different country that is known for poor prenatal care. Although the 1st child was born vaginally without complication, you have concerns that the 2nd child may be at risk for developing:
- Erythroblastosis fetalis
- Hereditary spherocytosis
- Hereditary elliptocytosis
- Polycythemia
- Pernicious anemia Answer A. When a Rh- mother is pregnant with her first Rh+baby, she is likely to develop IgM. ImgM is too large to cross the placental barrier and therefore will not affect the first child. However, upon becoming pregnant with a 2nd Rh+ babu, she will develop IgG which can cross the placental barrier and attack fetal erythrocytes. This condition causes erythroblastosis fetalis and can be fatal. This can be prevented by treating the mother with rhoGAM before or shortly after birth of first Rh+ baby. The patient in this question was likely not able to receive this treatment and therefore her 2nd baby will be at risk.
General Blood Histology & Hemopoiesis.
- Which of the following best describes the primary location of hematopoiesis during the 1st trimester, 2nd trimester and 3rd trimester during fetal development?
- Yolk sac → Liver → Bone Marrow
- Yolk sac → Spleen → Bone Marrow
- Liver → Yolk sac → Spleen
- Yolk sac → Bone Marrow → Liver
- Yolk sac → Bone Marrow → Spleen Answer A.
General Blood Histology & Hemopoiesis.
- An increase myeloid to erythroid ratio (e.g. 6:1) may indicate which of the following?
- Increased number of erythrocytes
- Decreased granulocytic cells
- Increased number of lymphocytes
- Increased number of monocytes
- InfectionAnswer E.
General Blood Histology & Hemopoiesis.
- A 12 year old female patient presents to the clinic complaining of joint pain, dizziness, fatigue, recurrent infections, and weight loss. Bone marrow aspiration reveals the presence of abnormal neutrophils, basophils, and eosinophils. Which of the following is the most likely diagnosis?
- Myeloid Lymphoma
- Lymphocytic Lymphoma
- Myeloid Leukemia
- Lymphocytic Leukemia
- Osteosarcoma Answer C.
General Blood Histology & Hemopoiesis.
- Psoriasis is a chronic skin condition caused by an overactive immune system. Symptoms include flaking, inflammation, and thick, white, silvery, or red patches of skin. Based on this knowledge, which basic function of the immune system is most likely impaired in a patient who has psoriasis?
- Cognitive Phase
- Activation Phase
- Effector Phase
- Immunological Memory
- Contraction Phase Answer E. The contraction phase involves the regulation of the effector functions to prevent immune-mediated damage to the body. In autoimmune diseases, this regulation is not functioning effectively allowing for an overactive immune system and consequential symptoms.
Immunology.
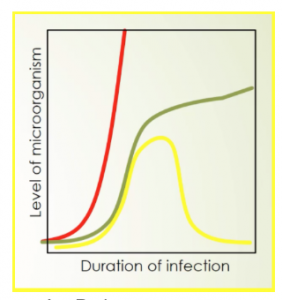
- Which of the following depicts deficient innate immunity in a host?

- Red
- Green
- Yellow
- Red & Green
- Green & Yellow Answer A.
Intro to Immunology.
- Which of the following is considered a primary lymphoid tissue?
- Lymph Node
- Spleen
- Liver
- Thyroid
- Thymus Answer E. Lecture #63 Intro to Immunology I.
- You are counselling your 5 year old patient’s parents on the importance of vaccinating. Which of the following basic immune function do vaccinations target?
- Innate Effector Function
- Adaptive Effector Function
- Innate Cognitive Phase
- Adaptive Memory
- Adaptive Cognitive PhaseAnswer D. Lecture #63 Intro to Immunology I.
- Which of the following correctly identifies the path of lymph through a lymph node?
- Afferent Lymphatic Vessel → Subcapsular Sinus → Cortex → Paracortex → Medulla → Efferent Lymphatic Vessel
- Afferent Lymphatic Vessel → Subcapsular Sinus → Paracortex → Cortex → Medulla → Efferent Lymphatic Vessel
- Afferent Lymphatic Vessel → Cortex → Paracortex → Medulla → Subcapsular Sinus → Efferent Lymphatic Vessel
- Afferent Lymphatic Vessel → Subcapsular Sinus → Medulla → Paracortex → Cortex → Efferent Lymphatic Vessel
- Afferent Lymphatic Vessel → Subcapsular Sinus → Medulla → Cortex → Paracortex → Efferent Lymphatic VesseLAnswer A. Lecture #63 Intro to Immunology I.
- A specific molecular moiety that has an antigenic determinant is a(n):
- Antibody
- Epitope
- Antigen
- TCR
- BCRAnswer B. Lecture 64, Slide #5. This might be too simple a question to appear on our actual exam, but we definitely need to understand the concept, and the difference between antigens and epitopes. Once you get the terminology down, think about the process an epitope is part of and what role it plays in the recognition phase of immune response.
- Which of the following is an INCORRECT statement regarding TCRs and BCRs:
- Only BCRs can recognize non-immunogenic molecules
- TCRs express MHC restriction
- BCRs are also called immunoglobulin
- TCRs recognize contiguous amino acid sequences
- Both BCRs and TCRs can be secreted to elicit an immune responseAnswer E. Lecture 64, Slides 6-9. This question may be too simple for the exam, but it should test whether you are picking up what Geis is putting down on a detail level. Also, if you understand how the receptors for B and T cells work, and how they differ, you can better understand the pathways they each effect.
- A 25 year old female patient presents with the cardinal signs of acute inflammation following a laceration to the right calf. You suspect she has developed a bacterial infection. Which of the following is true regarding her body’s immunological response?
- Her immune system is recruiting eosinophils and mast cells to combat the bacterial infection
- Her adaptive immune response is mediated by Th17 T-cells
- Her body is recruiting macrophages and natural killer cells to induce apoptosis, protecting her from the intracellular pathogen
- She is displaying Type II inflammatory response
- Her adaptive immune response is mediated by Th1 T-cellsAnswer B.
Inflammation.
- Neutrophilia is a blood condition characterized by high levels of neutrophils. Which of the following can be tested to confirm that a patient is displaying neutrophilia?
- Epo
- Tpo
- G-CSF
- M-CSF
- N-CSFAnswer C.
Inflammation.
- Which of the following is NOT associated with the inflammatory response to a helminth parasite?
- Eosinophils
- IL-5
- Mast Cells
- Th2 T-Cells
- Macrophages Answer E
Inflammation.
- A 3 year old male patient presents to the clinic with a history of recurrent bacterial infections and granulomas. A CBC indicates neutrophilia and you suspect Chronic Granulomatous Disease (CGD). Which of the following bacteria will be most detrimental to this patient?
- Catalase positive
- Catalase negative
- Facultative anaerobe
- Obligate anaerobe
- Gram positive Answer A. Individuals with CGD are deficient in the enzyme NADPH oxidase, which breaks down O2 into superoxide (which is eventually broken down into H2O2 by superoxide dismutase). The Neutrophil then creates bleach HOCl from H2O2 to combat bacteria. If the neutrophil is unable to create bleach, it cannot combat the bacteria. However, organisms that are catalase negative will be producing H2O2 but will be unable to break it down into H2O and O2. Therefore, the neutrophil will be able to “borrow” H2O2 from these bacteria to create HOCl and combat the bacteria. Organisms that are catalase positive will break down the H2O2 into H2O and O2 before the Neutrophil can “borrow” it to create the bleach needed to kill the bacteria.
Inflammation.
- Which of the following best describes a “left shift” in the inflammatory response?
- Le Chatelier’s principle drives the formation of banded cells to equilibrate with mature neutrophils
- Chronic granulomatous disease is caused by a deficiency in G-CSF causing an increase in immature neutrophils in the blood
- The appearance of immature banded cells in the peripheral blood indicating that the demands of the body to fight off a pathogen are exceeding the availability of mature neutrophils
- It occurs when a pathogen inhibits the production of mature neutrophils, resulting in an increase of banded cells in the peripheral blood
It is associated with an infection with C. trachomatisAnswer C. Inflammation.
- LAD is a genetic disease associated with a defect in leukocyte extravasation process, caused by a defective integrin. People with LAD suffer from recurrent bacterial infections and impaired wound healing. Which step in Leukocyte extravasation is impaired in individuals with LAD?
- Rolling
- Activation
- Diapedesis
- Chemotaxis
- AdhesionAnswer E.
Inflammation.
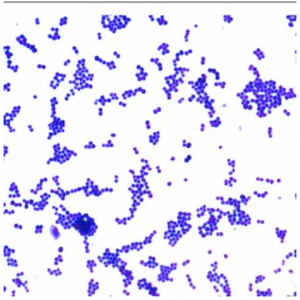
- The micropictograph below shows which of the following?

- Gram + Streptococci
- Gram + Staphylococci
- Gram – Streptococci
- Gram – Staphylococci
- Gram + Diplococci Answer B.
Basic Bacteriology.
- Which of the following is true of gram positive and gram negative bacteria?
- Gram positive bacteria stain pink
- Gram positive bacteria are composed of a lipid bilayer, separated by peptidoglycan
- Gram positive bacteria are more resistant to environmental changes than gram negative
- Gram negative bacteria have a thicker layer of peptidoglycan than gram positive bacteria
- Gram negative bacteria are all obligate intracellular Answer C.
Basic Bacteriology.
- A 15 year old male patient presents to the clinic with ear pain. Upon otoscopic examination, you notice that his tympanic membrane is red and inflamed and diagnose him with acute otitis media. Which of the following bacteria should you treat for?
- Haemophilus penumoniae
- Staphylococcus aereus
- Streptococcus pyogenes
- Streptococcus pneumoniae
- Chlamydia trachomatis Answer D.
Basic Bacteriology.
- An 86 year old female patient presents to the ED with cough, fever, chills, and difficulty breathing. You suspect pneumonia. Which of the following bacteria would NOT be a potential cause for this patient’s pneumonia?
- S. pneumoniae
- S. pyogenes
- H. influenzae
- S. aureus
- M. tuberculosisAnswer B.
Basic Bacteriology.
- Phenobarbital is a medication used to treat certain types of epilepsy in developing countries and has been known to increase levels of drug metabolism in mammals. One of the ways that phenobarbital elicits its effects is by regulating transcription of the cytochrome P450 gene. It is believed that this is accomplished when phenobarbital binds to cytochrome P450 and causes its dissociation from the DNA, allowing transcription to occur. Which of the following best describes the role that phenobarbital plays in this mechanism?
- Corepressor
- Effector
- Inhibitor
- Inducer
- Cofactor Answer D.
Prokaryotic Genetics.
- Which of the following is true when lactose is high and glucose is high?
- cAMP levels are high
- Allolactose binds to the repressor protein, allowing for transcription to occur at the Lac Operon
- Low levels of cAMP lead to increased formation of cAMP-CAP complexes
- The repressor protein is not being transcribed
- Allolactose binds to the activator protein, allowing for transcription to occur at the Lac Operon Answer B.
Prokaryotic Genetics.
- Which of the following would result in the highest level of transcription at the Lac Operon?
- Low glucose, high lactose
- High glucose, high lactose
- Low glucose, low lactose
- High glucose, low lactose
- Both A & BAnswer A.
Prokaryotic Genetics.
- Resistance of Staphylococcus aureus to antimicrobials has increased significantly over the past 40 years. Which of the following has most likely has contributed to this increase in resistance in Staphylococcus?
- Conjugation of the F plasmid
- Decreased plasmid relaxase
- Amplified exporter protein genes
- Conjugation of the R plasmid
- Increase transcription of the Lac OperonAnswer D.
Prokaryotic Genetics.
- Which of the following will result in a situation in which there is a transfer of donor bacterial DNA to recipient bacterial DNA and in which the exconjugant is converted to the donor state?
- F+ x F-
- Hfr x F-
- F’ x F-
- A & B
- A & CAnswer B.
Prokaryotic Genetics.
- Which of the will result in both a transformant and non transformant?
- Transduction
- Conjugation
- Mutation
- Transfiguration
- Transformation Answer E.
Prokaryotic Genetics.
- You’re making urea. You’re like woah cool a second amino group. Where that boi from?
- Aspartate
- Glutamate
- Malate
- Fumarate
- Ohnoimlate Answer A.
Amino Acid Metabolism.
- Carbamoyl phosphate synthetase I deficiency (CPS I deficiency) is an autosomal recessive metabolic disorder that causes ammonia to accumulate in the blood. A deficiency in which of the following cofactors is most likely to result in the same symptoms as a CPS I deficiency?
- Pyridoxine (B6)
- Biotin (B7)
- Cobalamin (B12)
- NAG
- Folate (B9)Answer D.
Amino Acid Metabolism I.
- A first year medical student is making rounds with the doc he is shadowing when they encounter a patient who presents with low iron levels in the blood. The doc explains to the medical about the internal mechanism humans have to regulate these iron levels. What is the best explanation?
- The ferrireductase enzyme uses ascorbate (vitamin C) to release more iron into the bloodstream
- Transferrin is upregulated and binds more Fe to export it into the bloodstream
- Hepcidin responds to either low or high iron levels by stimulating or degrading the ferroportin channel depending on the Fe levels
- Ferritin stores more Fe during low levels in order to prevent its release from the cell Answer C. Hepcidin stimulates Ferroportin to release more iron in low levels and degrades ferroportin preventing the release of iron in high levels.
Iron metabolism.
- What are the main causes of microcytic anemias?
- Thalassemia, sideroblastic anemia, chronic disease, iron deficiency
- Thalassemia, pernicious anemia, chronic disease, iron deficiency
- Thalassemia, sideroblastic anemia, acute diseases, iron deficiency
- Thalassemia, sideroblastic anemia, chronic disease, folate/B12 deficiencyAnswer A.
Iron metabolism.
- Hypochlorhydria is a deficiency of hydrochloric acid in the stomach. Stomach secretions are made up of hydrochloric acid, several enzymes, and a mucus coating that protects the lining of your stomach. A patient presenting which hypochlorhydria would most likely displaying symptoms of which of the following?
- Hemochromotosis
- Hypercalcemia
- Pernicious anemia
- Iron deficiency anemia
- Thalassemia Answer D. Lecture Iron Metabolism.
- There is a nasty bug going around the OMS I class! The trend has been students feel exhausted for a few days, then start to get a sore throat followed by headache, nasal drainage, and coughing (by day 3), and swollen lymph nodes (by day 5). It’s about 5 days of continuously feeling worse and worse before starting to feel better. Which of the following has most likely not yet occured by day three:
- Elevated IgM levels
- MHC II presentation on a dendritic cell
- B-Cell effector phase
- Binding of B-Cell MHC II with Th1 Cell IFN-gamma (TCR) in the lymph node cortex
- Migration of the mature, naive B-Cell to the follicleAnswer C. Lectures 64 and some of 65. To answer this question you need to understand the series of events that occur leading to the adaptive, cell-mediated and humoral response. Some of the following may happen simultaneously, but the final Effector Phase is always last, so this is the best answer to the question above.
- Your brain and also muscle is like whoa that’s a lot of ammonia. What enzyme most biggestly be like get atta heyah.
- Glutamate dehydrogenase
- Glutamine synthetase
- Glutaminase
- Alanine synthetase
- Alanine dehydrogenaseAnswer B.
Amino Acid Metabolism.
- Kuvan, at a cost of $100,000 per year for treatment of one patient, is used to supplement patients who are deficient in BH4. Deficiency in BH4 can mimic which disease state:
- PKU
- AKU
- Tyrosinemia
- Maple syrup urine disease
- AlbinismAnswer A. BH4 deficiency mimics PKU, causing hyperphenylalaninemia and a decrease in synthesis of catecholamines and serotonin.