- A 72 year old patient presents to the clinic complaining of shortness of breath, and fatigue. He is an avid smoker (1 pack a day for the last 30 years). He denies alcohol use. Upon examination, you note a systolic murmur heard best along the right eternal border in the second intercostal space. Which of the following are you most likely to see on an ECG (lead II)?
- Peaked P
- Bifid M shaped P wave
- ST Depression
- ST Elevation
- Absent P wavesAnswer B. Aortic Stenosis is a common cause of left ventricular hypertrophy and left atrial enlargement. Left atrial enlargement is shown on ECG as bifid M shaped P waves. Peak P waves are characteristic of right atrial enlargement and are unlikely to be shown in this patient. ST Elevation is indicative of MI and ST depression is indicative of ischemia. Left ventricular hypertrophy can cause Asymmetrical inverted T waves, Tall R (Leads I, aVL, V5, V6), and Deep S (Leads V1, V2)
ECG Chamber Enlargement.
You are concerned that a patient might have right atrial enlargement due to ongoing COPD. Which lead are you primarily going to analyze to determine if your suspicion is true?
- I
- III
- aVR
- V2
- V1Answer E. Lead II and V1 are primarily analyzed when looking for right atrial enlargement.
ECG Chamber Enlargement.
Which of the following is the most likely cause of right ventricular hypertrophy?
- Aortic Stenosis
- Systemic Hypertension
- Atrial septal defect
- Aortic Regurgitation
- Coarctation of the aorta Answer C. Atrial septal defect is a congenital heart defect that causes a left-to-right shunt between the atria. It is a common cause of RVH. While many of the answers could eventually lead to RVH if untreated, ASD is the most likely answer.
ECG Chamber Enlargement.
Which of the following is NOT a primary symptom of a right-to-left shunt?
- Polycythemia
- Clubbing of fingertips
- Cyanosis
- Hypoxemia
- Pulmonary hypertensionAnswer E. Examples of right-to-left shunts include tetralogy of Fallot, transposition of great Arteritis, persistent truncus arteriosus, tricuspid atresia, and total anomalous pulmonary venous connection. Pulmonary hypertension is a symptom of left-to-right shunts. It is also the reason for why left-to-right shunts will eventually become right-to-left shunts. Pulmonary hypertension will lead to thickening of the right side of the heart causing a reverse in pressure gradient (and eventual right heart failure). This is known as Eisenmenger syndrome.
Introduction to Cardiac Pathology I & II.
You are on rounds in OB-GYN when your attending calls you out to answer a question. She explains that the patient, a 2 week old female infant, is undergoing treatment with Indomethacin. Indomethacin is drug used to lower PGE2 levels. She also states that the patient is being treated for congenital Rubella. She asks you which congenital heart defect they are trying to correct with this medication. What is your answer?
- Atrial Septal Defect
- Ventricular Septal Defect
- Tetralogy of Fallot
- Patent Ductus Arteriosus
- Patent Foramen OvaleAnswer D. Patent Ductus Arterosus results from delayed closure of Ductus Arteriosus. The DA usually closes in response to declining PGE2 levels. While not in our lecture, it is extremely high yield (for boards) to know that this congenital heart defect is associated with congenital Rubella. Indomethacin is also a high yield for boards, but not discussed in our lectures.
Introduction to Cardiac Pathology I & II.
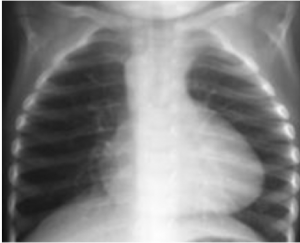
You are on rotations in OB-GYN where you are assisting in the delivery of a 3 week premature infant. Upon delivery, the infant has an APGAR of 6 and is displaying early cyanosis. Initial examination reveals a systolic murmur heard along the left sternal border in the 2nd intercostal space. After measures are taken to stabilize the infant, your attending orders a chest x-ray that is shown below. Which of the following is most likely the cause for the infant’s symptoms?

- Atrial Septal Defect
- Ventricular Septal Defect
- Tetralogy of Fallot
- Patent Ductus Arteriosus
- Patent Foramen OvaleAnswer C. Tetralogy of Fallot is composed of 4 features: Pulmonary stenosis, right ventricular hypertrophy, VSD, and Aorta overriding the VSD. This heart defect results in right to left shunting (causing early cyanosis) and a “boot shaped heart” (shown in the x-ray).
Introduction to Cardiac Pathology I & II.
Which of the following is a result of severe congenital aortic stenosis?
- Left Ventricular Hypertrophy
- Left Ventricular Hypoplasia
- Right Ventricular Hypertrophy
- Right Ventricular Hypoplasia
- Ventricular Septal Defect Answer B. CONGENITAL aortic stenosis/atresia will result in hypoplastic left heart syndrome. Unlike in aortic stenosis, the infant will have a hypoplastic LV. The left ventricle gains its size and function by pushing blood out of a compliant aortic valve. In this case, this can not happen so the ventricle does not form correctly. Tricuspid atresia will result in right ventricular hypoplasia.
Introduction to Cardiac Pathology I & II.
A 55 year old male patient presents to the clinic with a diastolic murmur best heard in the 5th intercostal space along the mid-clavicular line. Which of the following is most likely to be found in this patient’s history?
- Long History of Smoking
- Congenital Heart Defect
- Rheumatic Fever as a child
- Marfan Syndrome
- Familial History of MI Answer C. The question describes mitral stenosis which is almost exclusively caused by chronic rheumatic heart disease. Marfan syndrome is associated with mitral valve prolapse/regurgitation.
Introduction to Cardiac Pathology I & II.
Dilated cardiomyopathy (DCM) shows progressive cardiac dilation with poor contractile, resulting in systolic dysfunction. A positive test for which of the following would support a suspected diagnosis of DCM in a patient also denying alcohol use?
- Coxsackie A
- Streptococcus pyogenes
- Staphylococcus aureus
- Streptococcus viridans
- Parvovirus B19 Answer A. Coxsackie A and B (along with alcohol use) are highly associated with DCM.
Introduction to Cardiac Pathology I & II.
Which of the following occurs first in cardiac ischemia?
- Chest Pain
- Electrical Transit Abnormalities
- Regional Systolic Dysfunction
- Diastolic Dysfunction
- Myocardial necrosis Answer D. Diastole requires ATP
Ischemic Heart Disease.
What is the number one cause of cardiac ischemia?
- Prinzmetal’s angina
- Arterial thrombi
- Atherosclerosis
- Coronary emboli
- Congenital abnormalitiesAnswer C.
Ischemic Heart Disease.
Which of the following is NOT a component of atherosclerotic plaques?
- Subintimal collections of fat
- Smooth muscle cells
- Fibroblasts
- Intercellular matrix
- Elastic connective tissue Answer E.
Ischemic Heart Disease.
Which of the following post MI complications is likely to need a permanent pacemaker?
- Complete AV block due to inferior infarction
- Complete AV block due to anterior infarction
- Second degree AV block
- Atrial Flutter
- Supraventricular Arrhythmia Answer B.
Ischemic Heart Disease.
A patient presents to the Emergency Department with symptoms of an acute MI. Following treatment and examination, your attending asks you what the Killip classification of this patient is. You noted an S3 heart sound and rales in approximately 75% of the lung field. What is your answer?
- Class I
- Class II
- Class III
- Class IV
- Class VAnswer C. The Killip classification is a system used in individuals with an acute myocardial infarction, taking into account physical examination and the development of heart failure in order to predict and stratify their risk of mortality.
Class I – No S3 or rales
Class II – Rales in less than half the lung field
Class III – Rales in more than half the lunch field
Class IV – Cardiogenic shock
Ischemic Heart Disease.
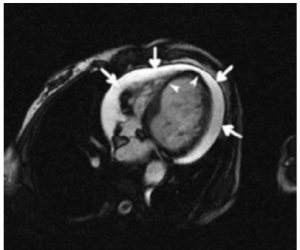
A 63 year old male patient presents to the clinic complaining of chest pain. He tells you that he is worried he is “having a heart attack again.” He was released from the Emergency Department only 2 weeks prior for an acute MI. Upon examination, you note a fever and friction rub. You perform a CT, which is shown below. What’s the diagnosis?

- Cardiogenic shock
- Ventricular aneurysm
- Ventricular septal rupture
- Dressler’s Syndrome
- Papillary muscle dysfunction Answer D. Dressler’s syndrome is a secondary form of pericarditis from a recent acute MI. Aspirin and oral corticosteroids are the treatment. Anticoagulants should be stopped. May also see pericardial effusion (shown on CT) but rarely tamponade.
Ischemic Heart Disease.
Which of the following is NOT a component of ACS management?
- Heparin
- Nitroglycerin
- ACE inhibitors
- Clopidogrel
- Calcium channel blockers Answer E. Know HOBANACS mnemonic. Heparin, Oxygen, Beta-blocker, Aspirin, Nitroglycerin, ACE inhibitor, Clopidogrel, Statins.
Ischemic Heart Disease.
Analyze the ECG below. Which of the following best describes your diagnosis?

- First Degree Heart Block
- Mobitz Type-I
- Mobitz Type-II
- 2:1 Block
- 3rd Degree Heart Block Answer C. PR intervals are unchanged and normal. However, not every P is followed by a QRS. Answers B, C, and D are all various types of Second Degree Heart Blocks.
ECG: Dysrhythmias.
Analyze the rhythm strip below (Lead II). Which of the following is your diagnosis?

- Normal Sinus Rhythm
- Sinus Bradycardia
- First Degree Heart Block
- Second Degree Heart Block
- Torsades de Pointe Answer C. A prolonged, unchanging PR interval is indicative of a first degree heart block.
ECG: Dysrhythmias
A patient comes in with complaints of heart palpitations feeling tired for the last several days. You order an ECG with the following results. With the patient’s history positive for asthma, which of the following medications would be best to correct the abnormality seen on ECG?

- Amiodarone
- Propafenone
- Mexiletine
- Lidocaine
- FlecainideAnswer E. This patient has sinus atrial fibrillation. Flecainide is indicated for supraventricular tachycardias, without the beta blocking activity that would make propafenone contraindicated. The other answer choices are all indicated for ventricular arrhythmias.
Anti-arrhythmic Agents I & II.
After a medical student collapsed due to finally getting back an exam score, they were taken to a nearby hospital, and required cardioversion to fix a dangerous arrhythmia. Within a few days of discharge, they began to experience severe headaches, nausea, and vomiting. They returned to the clinic with these symptoms along with complaints of a high-pitched ringing sound. Which drug was likely given to them that could have caused these symptoms?
- Quinidine
- Mexiletine
- Propafenone
- Esmolol
- DigoxinAnswer A. Quinidine should be discontinued when signs of cinchonism begin to manifest. Several of the other answer choices could cause the nausea, vomiting, and headaches, but tinnitus, hearing loss, and visual disturbances are more unique to quinidine.
Antiarrhythmic Agents I & II.
Which of the following scenarios would encourage you to perform an Echo in a newborn patient (24-48 hours of age)?
- POX of 90% on the right hand and 89% on left hand
- POX of 93% on right hand and 92% on the left hand
- POX of 90% on left root
- POX of 90% on the left foot and 95% on right hand
- None of the above would indicate the need for an echo Answer D. A difference between the right hand and either foot of >3% would indicate an echo is needed. The right hand or either foot should be between 90-95%. The left hand being lower than 90% would not necessarily indicate an echo. Due to the left subclavians proximity to the ductus arteriosus, it is frequently lower than the right hand. Remember that routine POX in the newborn (24-48 hours of age) is important to detect subclinical ductal-dependent cyanotic heart disease. In this disease, infants may appear pink but have a POX that is lower than normal.
Pediatric Cardio I & II.
You are performing a physical exam on a newborn patient. The patient is acyanotic but you notice a wide fixed splitting of S1-S2 and systolic murmur at the left 3rd intercostal space. You suspect an atrial septal defect, and perform an echo. You note an ASD on the inferior aspect of the interatrial wall, proximal to the endocardial cushion. Which of the following comorbidities is this patient likely to have?
- Down Syndrome
- Marfan Syndrome
- Congenital Rubella
- Rheumatic Fever
- Ventricular Septal DefectAnswer A. The question describes ASD of the ostium primum, which has a high occurrence rate among individuals with down syndrome. The ostium secundum defect will occur more superiorly on the interatrial wall.
Pediatric Cardio I & II.
You are on rotations in OB-GYN where you help to deliver a newborn baby girl. The patient is generally healthy in appearance, with an APGAR of 9 (some distal extremity cyanosis is present). Your attending assures you that this is relatively normal for most newborns. Heart sounds are normal. PMI is located in the 4th intercostal space along the left mid clavicular line and lung sounds are heard in all quadrants with no wheezing or crackles. However, you note that the patient is experiencing inspiratory dyspnea. What is the most likely diagnosis?
- Coarctation of the aorta
- Aortic Stenosis
- Ventricular Septal Defect
- Tetralogy of Fallot
- Double Aortic Arch Answer E. This patient is experiencing compression of the middle ⅓ of their trachea due to double aortic arch. Patients with this condition will be generally healthy but will experience breathing difficulties. In the lower ⅓ of the trachea the patient will experience wheezing, while in the middle/upper ⅔ of the trachea the patient will experience inspiratory dyspnea.
Pediatric Cardio I & II.
You are on rotations in OB-GYN when you help to deliver a newborn baby boy via cesarean section. The baby has an APGAR of 7 with severe cyanosis, weak cry, and low activity. Appropriate measures are taken to stabilize the infant and the nurse begins ventilation via BVM. Lab results show a substantial PaO2 difference between the right radial and umbilical arteries. You perform an echo which reveals interventricular flattening. Which of the following is a suitable treatment for this infant?
- Aspirin administration
- Blalock-Taussig shunt
- PGE2 administration
- Beta Blockers
- There is no treatment available Answer C. This patient most likely has Persistent pulmonary hypertension which results in severe cyanosis with tachypnea in absence of obvious pulmonary or cardiac disease. Treatment includes the administration of PGE2 to keep the PDA open. Treatment with inhaled nitric oxide (iNO) via mechanical ventilation is also used. Extracorporeal membrane oxygenation (ECMO) is yet another treatment used.
Pediatric Cardio I & II.
Which of the following is a common demographic for children diagnosed with Kawasaki Disease?
- Females
- Caucausin
- Hispanic
- Pacific Islander
- Black Answer D. KD is most common in males and asian/pacific islanders.
Pediatric Cardio I & II.
A 2 year old male patient presents to the clinic. The mother explains that the child has weird rash on his tongue and swelling in his hands and feel. Upon examination you also notice non-suppurative conjunctivitis and desquamation in the fingertips. The child has a fever of 101 ºF and an enlarged right anterior cervical lymph node. Which of the following lab results are you likely to find?
- Increased LDH
- Decreased ESR and CRP
- Markedly elevated Platelet count
- Decreased WBCs
- Increased RBCsAnswer C. This question describes Kawasaki disease which is typically associated with increased ESR/CRP, elevated platelets, and CSF pleocytosis. Treatment for this disease includes anti-inflammatory aspirin and IVIG. Do NOT give live attenuated vaccines when patient is on Aspirin (Reye’s Syndrome).
Pediatric Cardio I & II.
Which of the following is NOT part of the major Jones criteria?
- Migratory arthritis
- Carditis
- Erythema marginatum
- Subcutaneous nodules
- Fever Answer E. The Jones criteria is used in diagnosis of Rheumatic fever. Major criteria includes migratory arthritis, carditism erythema marginatum, subcutaneous nodules, and chorea. Minor criteria include arthralgia, fever, laboratory features, elevated ESR and CRP, prolonged PR interval.
Pediatric Cardio I & II.
A 25 year old female patient presents to the clinic with a decreased appetite, sudden weight loss, abdominal pain, excessive fatigue, and fever. She is also complaining heavily of a painful, pruritic, nodular like rash located on her legs that she believes to be unrelated. Her history is positive for Hepatitis B and Diabetes Mellitus Type I. Which of the following is likely affecting this patient?
- Giant Cell Arteritis
- Granulomatosis with Polyangiitis
- Eosinophilic Granulomatosis with Polyangiitis
- Polyarteritis Nodosa
- Kawasaki Disease Answer D. Polyarteritis Nodosa is associated with HBsAg and chronic Hepatitis B infection. It will affect the kidneys, heart, liver and GI tract. It will spare the lungs.
Intro to vascular pathology I & II.
A positive test for c-ANCA could confirm which of the following diagnoses?
- Giant Cell Arteritis
- Granulomatosis with Polyangiitis
- Eosinophilic Granulomatosis with Polyangiitis
- Microscopic Polyangiitis
- Kawasaki Disease Answer B. Eosinophilic Granulomatosis with Polyangiitis and Microscopic Polyangiitis are associated with p-ANCA while Granulomatosis with Polyangiitis is associated with c-ANCA.
Intro to vascular pathology I & II.
Which of the following can help you confirm a diagnosis of a tumor of endothelial origin?
- p-ANCA
- c-ANCA
- CD31
- CD55
- HBsAgAnswer C. Von Willebrand Factor can also usually confirm endothelial origin.
Intro to vascular pathology I & II.
A 32 year old male patient presents to the clinic with concerning cutaneous red-purple plaques on his foot. He has a history of HIV. Which of the following are likely to be positive?
- p-ANCA
- CD55
- CD31
- HBsAg
- HHV-8 Ag Answer E. This patient most likely has Kaposi sarcoma, a vascular neoplasms caused by HHV-8 and highly associated with AIDS.
Intro to vascular pathology I & II.
You are seeing a 23 year old man in the ED who is complaining of sudden onset severe substernal pain that has begun to radiate to his back which began at rest. His respiratory rate is 28 and he is having difficulty staying alert. Initial labs show normal troponin.What test would give you the best chance of immediately confirming your diagnosis?
- TEE
- Abdominal CT with contrast
- ECG
- Renal Angiography
- CXRAnswer A. This man has an aortic dissection, evidenced by the severe acute chest pain radiating to the back. Aortic dissection also causes SOB and syncope. TEE (transesophageal echo) is the best method out of these options to diagnose this condition. MRI and chest CT could also be used. Option B would be used to detect AAA. C would be for suspicion of MI, although his age and the sudden onset would make this less likely, and TEE would be a next step if ECG came back abnormal. Renal angiography would be if it were suspected secondary HTN. CXR could detect dissection, but 1/3 of CXR fail to show dissection and it requires a well trained eye to use this modality effectively. This isn’t in our content but is a high yield board concept!!!
Atherosclerosis.
A 58 year old male patient presents to the clinic for a health exam. He is feeling generally healthy and has no complaints besides his typical symptoms of osteoarthritis in his hands. History is positive for a 30 pack year. You are palpating his abdomen when you feel a large, periumbilical, pulsatile mass. You order imaging which shows a 3cm AAA, confirming your diagnosis. Which of the following is TRUE regarding this individual?
- Surgery is not indicated at this time since the patient’s risk for rupture is virtually non existent
- This patient needs timely surgery to prevent imminent rupture
- This patient has an 11% annual risk of rupture
- This patient has a 25% annual risk of rupture
- This patient has a 1% annual risk of rupture Answer A. AAA less than 4cm has a nil risk of rupture and surgery should not be performed.
Atherosclerosis.
Which of the following is INCORRECT regarding aortic aneurysms and dissections?
- Hypertension is the major risk factor for ascending aortic aneurysm
- Marfan syndrome is often associated with aortic dissections
- Ehlers Danlos is often associated with aortic dissections
- Atherosclerosis is the major risk factor for abdominal aortic aneurysms
- Infective endocarditis is highly correlated with aortic dissections Answer E. Infective endocarditis is associated with mycotic aneurysms (affecting cerebral vasculature and sometimes the aorta). This one’s kind of tricky since there are subtleties between aneurysm and dissections, but study the answer choices because we are likely to get a question on one of concepts.
Atherosclerosis.
One of your patients with a history of endocarditis has called you to ask for prophylactic antibiotics preceding a root canal in the near future. He is positive for allergies to beta lactam antibiotics and has difficulty with some medications due to age and progressing Parkinson’s disease. What would be an appropriate prescription for this patient?
- Amoxicillin PO 1h before procedure
- Ampicillin 2g IV 1hr before procedure
- Clindamycin 600mg IV 1hr before procedure
- Cephalexin 2g PO 1hr before procedure
- Clarithromycin 500mg PO 1hr before procedureAnswer C. The stem gives that this patient has an allergy to beta lactam drugs (penicillin). This eliminates options A and B immediately. The next concern is the patient’s ability to take oral medications. 50% Parkinson’s patients report dysphagia, which is also an issue with many elderly patients. Giving an IV or IM drug would then be preferred. This would rule out choices D and E.
General Valvular Disease I & II.
Which symptom, when paired with the presence of carditis and evidence of GAS infection, is NOT sufficient for a diagnosis of ARF?
- Chorea
- Elevated ESR and CRP
- Subcutaneous nodules
- Polyarthritis
- ChoreaAnswer B. Elevated ESR and CRP are minor Jones criteria for ARF. Diagnosis would require a second minor criteria, along with the stated major criteria of carditis. All other answer choices are major criteria, which alongside carditis would be sufficient for diagnosis of ARF.
General Valvular Disease I & II.
A 56 year old man who you have seen for years comes in for a wellness check. He has a blood pressure of 140/80 and has been on medication for his HTN for years. For the past few weeks he has been complaining of difficulty with urination, with a stream that starts and stops. Following your suspicions, you receive a positive blood test for a specific tumor biomarker. What drug could you replace his current HTN medication to help with his newly onset symptoms?
- Captopril
- Losartan
- Methyldopa
- Nifedipine
- DoxazosinAnswer E. Doxazosin is indicated for treatment of benign prostatic hyperplasia as well as hypertension. The “stop and start” urine stream and difficulty with urination, as well as frequency of urination, are signs of BPH. A positive prostate specific antigen (PSA) blood test would help to diagnose this condition. Blockage of the alpha 1 receptors by doxazosin help to limit the proliferation of prostatic tissue.
A patient comes into the clinic for a follow-up 7 days after being discharged from the hospital following an acute myocardial infarction. The patient is complaining of feeling tired throughout the day and being short of breath when they exert themselves. They have also been unable to perform with their partner. ROS is negative for arthralgia or muscle pain. Which of the following medications is most likely the cause of their symptoms?
- Lisinopril
- Atenalol
- Clopdigrel
- Atorvastatin
- VerapamilAnswer B. Atenalol is a beta blocker indicated for MI patients and can cause fatigue, bronchoconstriction, and sexual dysfunction. The other answer choices are also given to patients with an MI to reduce risk of cardiac death, but do not cause the symptoms the patient has complaints with. The best distractor would be atorvastatin, which can cause all of the patient’s symptoms other than incompetence, but is usually associated with joint and muscle pain.
You are attempting to treat a patient with hypertension who has a history of asthma. Which of the following drugs would be most appropriate to prescribe initially?
- Atenolol
- Amiodarone
- Captopril
- Aliskiren
- Clonidine Answer C. Beta-blockers are contraindicated in patients with asthma, ruling out answers A & B. Aliskiren and Clonidine do treat HTN, but should not be your first go to. ACE inhibitors/ARBs would be your best choice. Captopril is an ACE inhibitor.
Which of the following drugs is NOT associated with torsades de pointe as a side effect?
- Disopyramide
- Quinidine
- Procainamide
- Dofetilide
- Sotalol Answer A. Drugs that may cause Torsades de Pointe include Sotalol, Amiodarone, Dofetilide, Procainamide, Quinidine, and Ibutilide. Magnesium Sulfate is the treatment for Torsades de Pointe.
Which of the following drugs is used to treat bradycardia?
- Adenosine
- Digoxin
- Atropine
- Magnesium Sulfate
- Captopril Answer C.
A 75 year old male patient presents to the clinic for a wellness check. He has a history of diabetes mellitus that he states has been well controlled with diet and use of Metformin. Last time you saw him, you diagnosed him with HTN which you prescribed Lisinopril to control. Although this patient has been taking his medications religiously, his blood pressure is still reading slightly high at 146/88. You decide to prescribe an adjuvant drug. Which drug would you want to AVOID giving to this patient?
- Valsartan
- Losartan
- Methyldopa
- HCTZ
- AliskirenAnswer E. Aliskiren is contraindicated in diabetic patients with an ACE or ARB.
A 75 year old male patient presents to the clinic for a wellness check. He has a history of diabetes mellitus that he states has been well controlled with diet and use of Metformin. Last time you saw him, you diagnosed him with HTN which you prescribed Lisinopril to control. While his blood pressure has been well controlled since, he is complaining of a persistent cough. Which of the following drugs would you replace with lisinopril to reduce this side effect?
- Losartan
- Methyldopa
- HCTZ
- Aliskiren
- Fosinopril Answer A. Cough and angioedema is less associated with ARBs. The other drugs (while not associated with cough) should not be considered without trying an ACE and ARB first.
- A 58 year old female presents to the ER complaining of general fatigue/weakness, numbness, and nausea/vomiting. History reveals a history of hypertension, which has been controlled with a medication she can’t seem to remember the name of. She notes that she had been having a history of painful leg cramps a couple months back. Her friend recommended taking potassium supplements over the counter to help. Based on this information, which of the following drugs is this patient most likely taking to control her hypertension?
- Methyldopa
- HCTZ
- Aliskiren
- Candesartan
- Clonidine Answer D. ACE inhibitors and ARBs can cause hyperkalemia when used in conjunction with potassium supplements or potassium sparing drugs.
- A patient with Pheochromocytoma would most benefit from which combination of drugs to control HTN?
- Phenoxybenzamine and Procainamide
- Phenoxybenzamine and Propranolol
- Phenoxybenzamine and Doxazosin
- Procainamide and Doxazosin
- Procainamide and ProzosinAnswer B. Phenoxybenzamine and Propranolol are often used in conjunction to treat Pheochromocytoma.
- Which of the following drugs are contraindicated with the administration of Nitroglycerin?
- Aspirin
- Morphine
- Viagra
- Losartan
- CholestyramineAnswer C. Erectile Dysfunction drugs are contraindicated with use of Nitro.
Pharmacological Management of Angina and CAD.
- Which drug is best for the treatment of Type III hyperlipoproteinemia?
- Gemfibrozil
- Ezetimibe
- Alirocumab
- Lomitapide
- Mipomersen Answer A.
- A 63 year old man is at dinner. When he is chewing his food, he begins to feel like he has a headache. He arrives at the clinic and your workup shows an elevated ESR. Your biopsy shows the following:

What is your diagnosis?- Giant Cell (Temporal) arteritis
- Takayasu arteritis
- Kawasaki Disease
- Polyarteritis Nodosa
- Churg-Strauss SyndromeAnswer A. Jaw claudication is a common sign of temporal arteritis as well as an elevated ESR. Temporal arteritis is intimal thickening and fragmentation of large vessels.
- Which of the following serology components is found in a 37-year-old with polyarteritis nodosa?
- Heterophile antibodies
- Positive dsDNA antibodies
- Positive p-ANCA
- Hepatitis B surface antigens
- Antibodies to basement membraneAnswer D. 30% of PAN patients have chronic Hepatitis B with depositis of HBsAg-HBsAb complexes in affected vessels.
- A 62 year old man presents complaining of shortness of breath and mild chest pain when walking up the stairs at his apartment for the past 2 months. He does not have any significant prior medical history. On exam, you note a 2/6 holosystolic murmur at the 5th intercostal space to the left of the sternum. Which of the following is the correct murmur.
- Mitral Stenosis
- Mitral Regurgitation
- Aortic Stenosis
- Aortic Regurgitation
- Mixed Mitral Valve Disease Answer B.
- A 24 year old female with a history of hypertension presents with symptoms of hypokalemia. She is currently taking an ACE inhibitor for hypertension control. Following laboratory testing, you notice her aldosterone is elevated and she is hypokalemic. You discover the underlying cause of they hyperaldosterinism is most likely due to an adrenal gland tumor. Which drug will you administer to this patient?
- Acebutolol
- Spironolocatone
- Valsartan
- Aliskiren
- Lisinopril Answer B. In normokalemic or hyperkalemic patients, spironolactone is contraindicated due to it being a potassium-sparing drug; however, in this case, the patient is hypokalemic, so giving spironolactone would actually be beneficial.
- Which of the following is TRUE regarding Cysticercosis?
- You can only get it from eating undercooked pork
- It’s caused by T. sanginata.
- It results in elephantiasis
- Its a relatively asymptomatic disease
- It can cause cysts in the brainAnswer E.
Micro Review,